
Medical terms can feel confusing, especially when they sound almost the same. Imagine, for example, hearing phrases like 'cervicitis' or 'cervical erosion' during a visit to the doctor. It’s quite easy and natural to mistake one for the other. Many people go through situations like this, even during routine appointments.
It’s essential to learn to differentiate between these two illnesses, since their symptoms, causes, diagnostic methods, and treatments are quite different. In this article, we aim to provide greater clarity on these two medical terms.
The term 'cervical erosion' can sound alarming, but it is often misleading. Nothing is actually eroded or damaged. Cervical erosion, also called cervical ectropion, occurs when cells from the inner part of the cervix appear on the outer surface. This occurs when the cervix turns slightly outward, exposing the inner lining.
The cervix contains two types of cells. The outer part is covered with flat, pale-pink squamous cells, similar to the lining of the mouth. The inner part is lined with glandular cells that have a softer, more textured appearance. In cervical erosion, these glandular cells are seen on the outside of the cervix.
This is a common and harmless variation in the way cervical cells appear. It is not a sign of cervical cancer or another serious health condition.
Cervical ectropion is more common during the reproductive years and uncommon after menopause. It tends to occur when estrogen levels are higher. This makes it more likely during adolescence, pregnancy, and around ovulation in the menstrual cycle. The condition is also more common in those using estrogen-progestin contraceptives. A cervix that has been stretched or torn during childbirth may also be more prone to developing cervical ectropion.
Women may have cervical ectropion from birth or develop it later in life. It most often appears when hormone levels change and estrogen levels rise. This commonly happens during puberty, pregnancy, or while taking birth control pills that contain hormones. These hormonal shifts influence the positioning of cervical cells, making the inner cells more visible on the outer surface.
Cervical ectropion often causes no symptoms. In many cases, cervical erosion symptoms are noticed only during a routine pelvic exam or a Pap smear. Because it is a harmless condition, it may not even be mentioned during the visit.
In a small number of cases, mild symptoms can occur. These include changes in vaginal discharge, which may appear bloody or mucus-like. Some people notice light bleeding or discomfort during or after intercourse, or slight bleeding during a pelvic exam. Occasional spotting between periods or pelvic discomfort may also be present. These signs are usually mild and are often linked to other conditions rather than cervical ectropion itself.

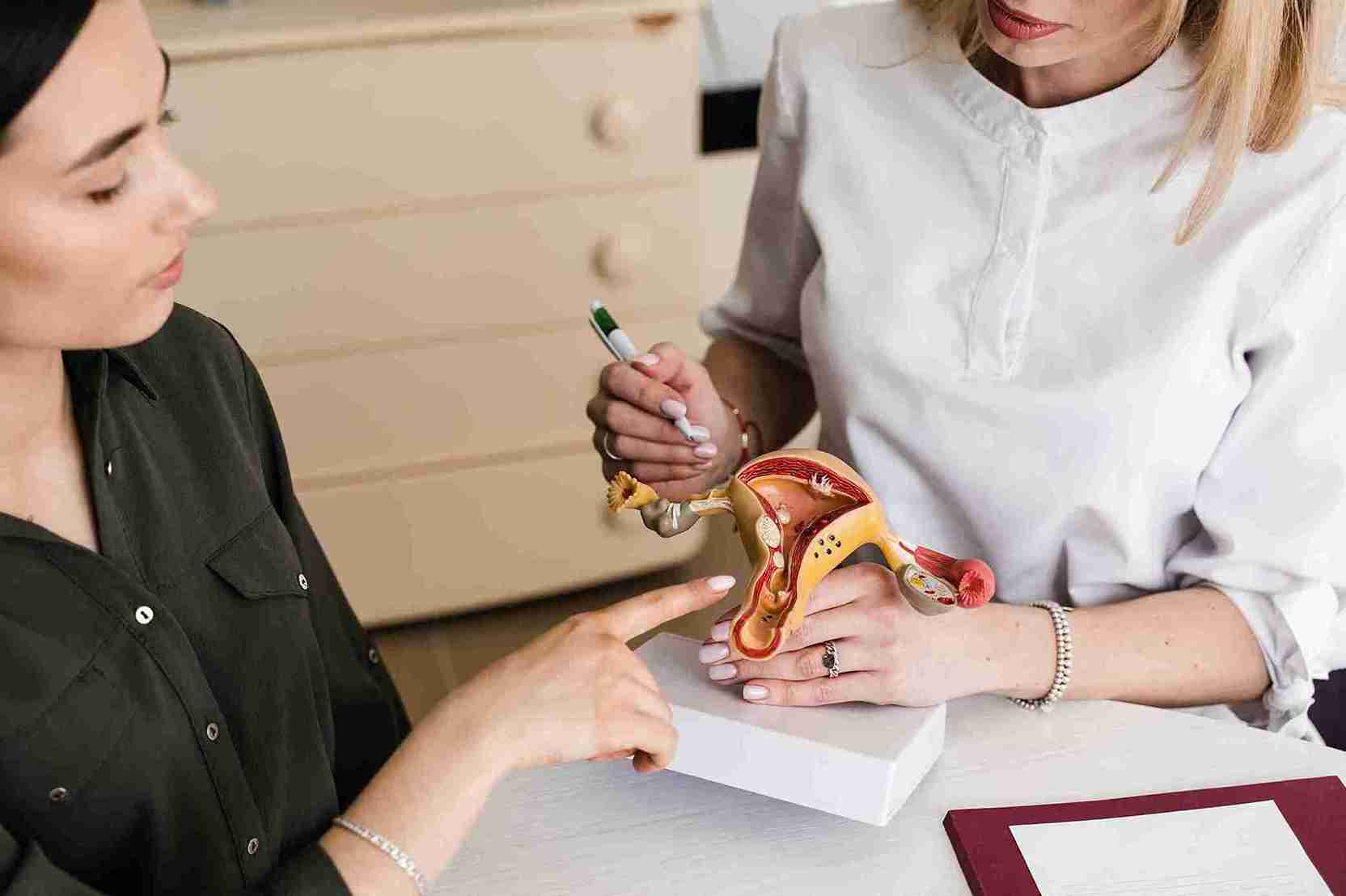
Cervical ectropion is usually identified during routine checks. Your doctor may use one or more of the following methods.
The cervix and other reproductive organs are examined to look for visible changes.
Cells from the cervix are collected to rule out precancerous changes.
A special lighted tool helps the doctor view the cervix more closely.
A small tissue sample may be taken to examine cervical cells in detail and exclude serious conditions.
In most situations, there is no need for cervical erosion treatment. Medicines may be prescribed to manage frequent vaginal discharge or spotting. In severe cases, treatments like diathermy or cryotherapy may be used to destroy the abnormal cells.
Cervicitis is different from cervical erosion and should not be confused with it. Unlike erosion, cervicitis involves inflammation of the cervix. This inflammation matters because, if left untreated, it can lead to complications such as pelvic inflammatory disease. PID can cause scarring in the uterus, ovaries, or fallopian tubes, which raises the risk of long-term pelvic pain, infertility, or ectopic pregnancy. An inflamed cervix also allows bacteria and viruses to enter the body more easily, increasing the risk of sexually transmitted infections, including HIV.
● Acute cervicitis is a condition that starts suddenly. Bacterial infections, including sexually transmitted infections, cause most cases. Symptoms tend to feel more noticeable, and this form can be passed to sexual partners.
● Chronic cervicitis, on the other hand, is a condition that lasts for months. Symptoms stay mild or go unnoticed. It usually results from irritation rather than infection. Triggers include reactions to feminine products, latex condoms, etc.
Cervicitis is not usually life-threatening, and it can be easily managed or treated.

Most cases of cervicitis occur in people with a history of sexually transmitted infections. Therefore, having multiple partners or engaging in unprotected sex could increase the risk of getting this disease.
Cervicitis has different causes based on whether it is acute or chronic.
Sexually transmitted infections are typically the cause of acute cervicitis. Gonorrhoea, genital herpes, trichomoniasis, and chlamydia—which causes the majority of cases of cervicitis—are common causes.
Chronic cervicitis is typically not linked to sexually transmitted infections. It often results from irritation in the vaginal area. Triggers include reactions to spermicides, douches, or latex condoms, sensitivity to items placed inside the vagina, such as tampons or diaphragms, etc.
The symptoms of cervicitis are similar to those of other disorders, such as vaginitis or a yeast infection, which is why it is recommended to get regular STI screenings and gynaecological exams to rule out cervicitis if any of the following symptoms are noticed.
● Abnormal vaginal discharge that has a yellow, grey or white colour. It may look like pus and could have an unpleasant smell.
● Irritation or itching.
● Abnormal light vaginal bleeding or spotting.
● Dyspareunia or painful sexual intercourse.
Cervicitis is usually diagnosed after conducting a pelvic exam. A gynaecologist will look for pus-like vaginal discharge or any unusual redness or inflammation in the cervix and vaginal walls. A cotton swab will be used to gather a sample of vaginal discharge, which will be forwarded to the laboratory for infection detection.
Infections causing cervicitis can be treated with antibiotics or antivirals, depending on the pathogen. Cervicitis caused by allergic reactions tends to resolve once exposure to the allergens ceases.

This article, which explores cervical erosion vs. cervicitis, highlights the importance of distinguishing between similar-sounding terms that refer to very different cervical conditions. This kind of awareness helps clear confusion and makes health information easier to understand.
Recommend regular Pap smears with HPV DNA testing yearly in All Ladies for reproductive age group and above
HPV vaccination to all above 10 years of age. Dose recommended as per age

Cervical erosion is usually diagnosed via a pelvic exam, biopsy, colposcopy, or Pap smear.

Cervical erosion is usually harmless and is not indicative of cancer.

Cervical erosion may lead to the occurrence of white vaginal discharge.

In the majority of cases, fertility or pregnancy is unaffected by cervical erosion.