
For many couples, the dream of having a child can be filled with joy, but for some, the journey to conception and carrying a pregnancy to full term can be complicated. One such condition that can make this dream difficult to achieve is Asherman’s Syndrome. Understanding the causes and risk factors of Asherman’s syndrome is crucial for women who may be struggling with unexplained fertility issues or recurrent miscarriages, as it can offer insight into potential treatments and solutions. In this article, we shall take a closer look at this disorder.
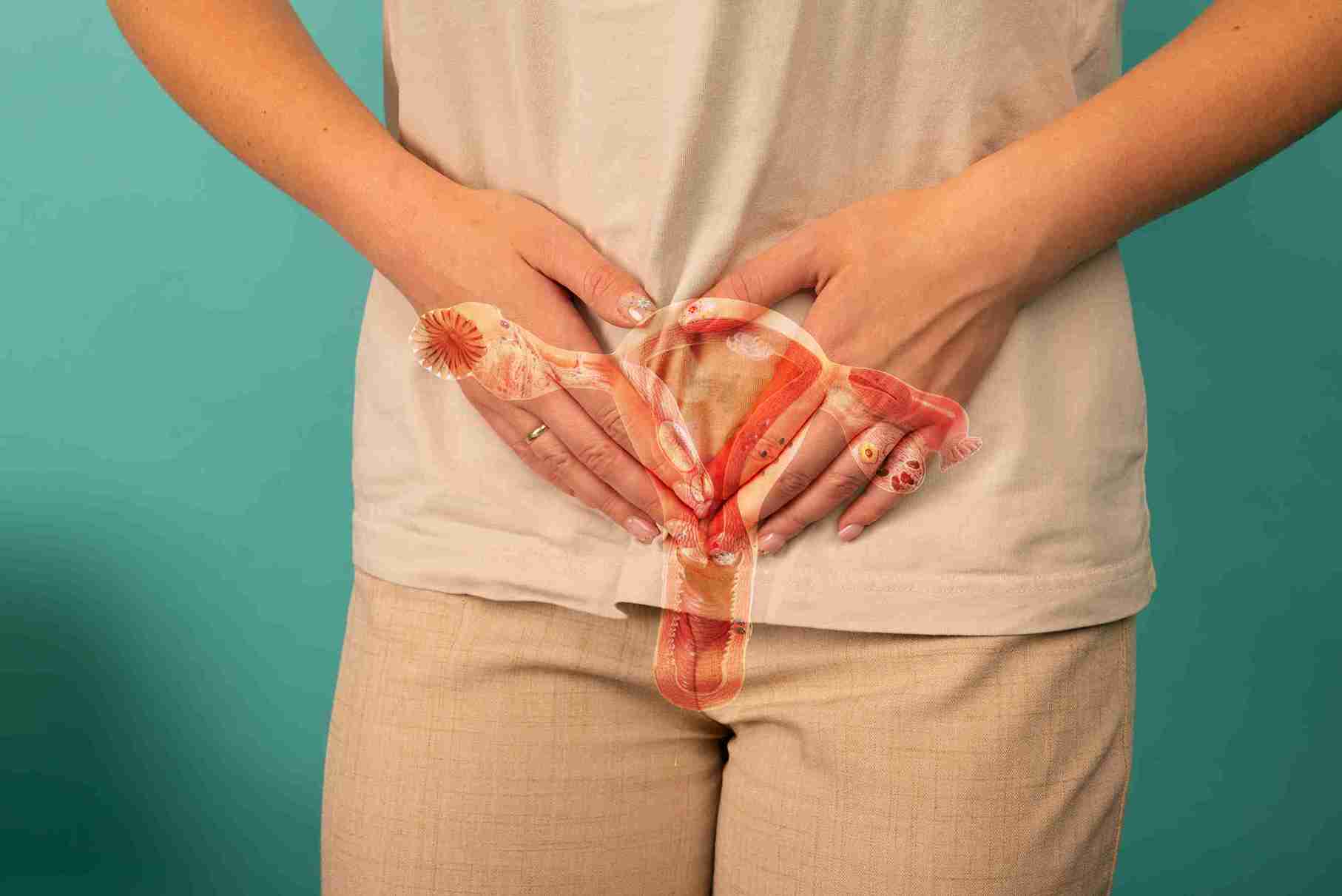
Asherman’s syndrome, also known as Fritsch-Asherman syndrome, is a rare gynaecological disorder. The main feature of this disorder is the creation of uterine scar tissue, also known as adhesions or intrauterine adhesions, in the uterus. This extra tissue grows to such an extent that it takes up most of the space in the uterus, and it may be thick or thin. These adhesions may sometimes block the cervix. In mild cases, the adhesions will be fewer and seen in only a few areas of the uterus. However, in severe cases, the adhesions will be widespread and may cause the walls of the uterus to stick together, partially or completely.
The presence of scar tissue in the uterus may give rise to several complications, especially for women who are trying to conceive. Apart from fertility issues, Asherman’s syndrome increases the chance of miscarriage or stillbirth, as the presence of scar tissue leaves no room for the baby to grow in the uterus. Asherman’s syndrome could also cause placenta previa, whereby the placenta’s position is relatively low in the uterus. This could create problems during delivery as the placenta could end up blocking the cervix, thus preventing the baby from moving out of the uterus.
Hence, it is vital to recognise the signs and symptoms of Asherman’s syndrome so that treatment options may be explored as soon as possible.
● Abnormal or irregular uterine bleeding
● Amenorrhea or absence of menstruation
● Hypomenorrhea or abnormally light menstrual bleeding
● Severe cramping or pain in the pelvic region
● Fertility issues that prevent conception or carrying the baby to full term.
It is recommended to consult a gynaecologist if any of the above signs have been noticed.
They can use diagnostic tests to identify the cause and begin treatment if needed. Diagnostic tests can help determine the cause, allowing for the start of treatment if necessary.

1. Dilation and Curettage (D&C)
Dilation and curettage (D&C) is a standard medical procedure. The cervix is dilated or expanded, and a special spoon-shaped tool called the curette is used to carefully scrape and remove any abnormal tissue from the uterus’s lining. This procedure helps remove the tissue left from an incomplete miscarriage or from the placenta that remains in the uterus after childbirth or during an elective abortion. A D&C usually causes no scarring or endometrial damage unless there is an underlying infection that wasn’t noticed before or during the procedure.
2. Operative Hysteroscopy
A hysteroscopy is a minimally invasive procedure that may be combined with a D&C procedure. During a diagnostic hysteroscopy, a doctor will insert a camera into the uterus and use it to view the uterus’s lining to detect the presence of any uterine disorders. Once any abnormal tissue or growth, such as polyps, fibroids, etc., is detected, operative hysteroscopy will be performed to remove it. Poorly performed operative hysteroscopy could damage the endometrial tissue and cause scarring.
3. Cesarean Section (C-section)
Sometimes, C-section surgeries could also be a cause for the development of scar tissue in the uterus. This typically happens when there is an undiagnosed infection, usually at the site of the sutures or stitches. Such infections could lead to scarring of the uterine tissues.
4. Radiation Treatment
The treatment of certain diseases, like cervical cancer, requires the use of radiation therapy. Such treatments, where there is prolonged exposure to radiation, could cause adhesions to form, thus leading to Asherman’s syndrome.
5. Infections
Infections like cervicitis and pelvic inflammatory disease (PID) can also lead to Asherman’s syndrome.
Asherman’s syndrome is an acquired and not a hereditary or genetic disorder. This means that Asherman’s syndrome is not passed from one generation to the next. Instead, it occurs due to medical procedures or infections that trigger the creation of scar tissue or adhesions.
IUDs have not been proven to be a major cause of Asherman’s syndrome, even though their usage could potentially lead to infections and the formation of adhesions.
Asherman’s syndrome is a rare condition, but certain women may be more likely to develop it. Those at higher risk include:
● Women who have undergone procedures like D&C, operative hysteroscopy, etc.
● Women who have delivered via C-section.
● Women who have undergone radiation therapy for treating cancers of the cervix.
● Women with a history of pelvic infections.

As stated earlier, Asherman’s syndrome is a rare disorder, and its symptoms are similar to those of other health conditions. Usually, the doctor examines the medical history carefully and recommends getting a few blood tests or physical examinations to rule out other conditions.
Once this has been done, and there is a strong suspicion of Asherman’s syndrome, the doctor may recommend further tests. Usually, any of the following tests may be recommended to detect the presence of scar tissue:
1. Ultrasound
Ultrasound imaging may be performed, either externally or internally, to create an image of the uterus. This allows the healthcare provider to view the thickness of the lining of the uterus and the follicles.
2. Hysteroscopy
A hysteroscopy procedure may be performed, as it allows the doctor to view the inside of the uterus in detail and find out if there are any adhesions or scarring.
3. Saline Infusion Sonography
Saline infusion sonography is a type of ultrasound that uses saline, a salt and water mixture. Using a small catheter, the saline mixture is injected into the uterus to expand it, thereby allowing the doctor to use transvaginal ultrasound to create a detailed image of the uterus.
Once Asherman’s syndrome has been diagnosed, the doctor will recommend treatment based on the medical history and overall health of the woman.
If a hysteroscopy was performed for detecting Asherman’s syndrome, then the doctor may perform operative hysteroscopy to slowly and carefully remove the scar tissue. While this procedure is generally safe, there is a risk of accidentally removing or damaging healthy tissue during this procedure. Antibiotics will be prescribed to minimise the chance of infections.
Along with hysteroscopy, hormonal treatments using estrogen may also be recommended. Estrogen helps in healing the endometrium. A small intrauterine catheter may be placed in the uterus along with estrogen. The catheter creates a barrier between the posterior and anterior walls of the uterus, thus ensuring that they do not stick to each other after the scar tissue has been removed.

Asherman’s syndrome is an uncommon health issue that could affect fertility. Women with Asherman’s syndrome have scar tissue or adhesions in their uterus. This scar tissue could fill up the space within the uterus and prevent the conception and development of a fetus in the uterus.

Asherman’s syndrome is an acquired disorder. This means it occurs due to medical or surgical procedures, radiation therapy or infections like PID.

Uterine scarring leads to the creation of scar tissue called adhesions. The presence of such adhesions is one of the main signs of Asherman’s syndrome.
